Screening of medical problems in adults with Down syndrome
Two-hundred and one adults with Down syndrome, living in the hospital and community, were assessed to ascertain prevalence of medical problems. Eighty-one percent of individuals examined were found to be overweight or obese (BMI >24), significant impaired vision was present in 18% and significant impaired hearing in 12%. A further 12% had a cardiac murmur and 15% of males had an undescended testis. Flat feet were found in the majority of subjects (70%) with xerosis in over a third of subjects (39%). A low heart rate and low blood pressure recordings were typical findings. A history of epilepsy was found in 8% of subjects. Particular concern needs to be given to obesity, sensory impairment and thyroid dysfunction and regular screening of all adults with Down syndrome is recommended.
Prasher, V. (1994) Screening of medical problems in adults with Down syndrome. Down Syndrome Research and Practice, 2(2), 59-66. doi:10.3104/reports.31
Introduction
The health of people with Down syndrome has, until recently, been of low priority. During the early part of this century admission of individuals with Down syndrome to long stay institutions meant that these problems were hidden away, out of sight and out of mind. With the recent increase in public awareness and support from the Government and the publication of "The Health of the Nation" document (Department of Health, 1992), there is now the potential for change, and people with Down syndrome may expect the same level of healthcare and quality of life as the rest of the population.
Further, adults with Down syndrome are living longer than previously and individuals surviving into their sixth or seventh decade of life are now encountered (Baird and Sadonivick, 1988; Prasher, 1993). With increased longevity, such individuals are susceptible to differing medical and psychiatric disorders, including visual impairment (Caputo, et al, 1989; Hestnes et al, 1991), hearing loss (Yeates, 1992; Evenhuis, 1992), thyroid dysfunction (Pueschel and Pezzullo, 1985; Dinani and Carpenter, 1990), dementia (Oliver and Holland, 1986; Prasher and Krishnan, 1993) and depression (Collacott and Cooper, 1992; Burt et al, 1992). Consequently there is a need for an overall assessment of the health of adults with Down syndrome.
Evidence demonstrating the need for an assessment of medical problems for adults with Down syndrome is available from two sources; findings for people with learning disability as a whole (Jacobson and Janicki, 1985; Wilson and Haire, 1990) and from findings for children with Down syndrome (Howells, 1989; Cooley and Graham, 1991). However, extrapolation of findings from these groups to adults with Down syndrome is inappropriate and likely to be inaccurate.
Certain disorders are specifically associated with adults with Down syndrome, e.g. cataracts, and therefore under-represented in other groups. It is important for adults with Down syndrome to be assessed as an independent group. The author is unaware of any large scale study of adults with Down syndrome investigating rates of different physical disorders present in this population. This research study investigates this important area of research.
Methodology
Adults with cytogenetically and/or clinically proven Down syndrome were recruited for the study. Both community residents, living in their family home or in small community units, along with hospital residents were assessed. Severity of learning disability was assessed by review of previously reported intelligence tests' results, previous level of functioning as determined by review of medical notes, from carer interview and from mental state examination of the individual. Severity of learning disability was classified using ICD-10 criteria (WHO, 1992).
For each individual, carers were interviewed to elicit a past history of any medical condition and to elicit any symptoms suggestive of an ongoing medical illness. Previous hospital records and, where necessary, general practitioner records were reviewed to confirm the existence of a past or present disorder. All individuals were interviewed and again, a history taken to elicit any symptomatology suggestive of any medical disorder. Medication prescribed was recorded.
| Past Disorder | Frequency | |
|---|---|---|
| Cardiovascular | varicose veins | 3 |
| Fallot's tetralogy | 1 | |
| Respiratory | recurrent infections | 15 |
| asthma | 1 | |
| Abdominal | peptic ulcer | 3 |
| constipation | 2 | |
| Coeliac disease | 1 | |
| Hirschsprung's disease | 1 | |
| Oesophageal stricture | 1 | |
| Genitourinary | prostate pathology | 2 |
| inguinal hernia repair | 2 | |
| nephrectomy | 1 | |
| partial amputation penis | 1 | |
| circumcision | 1 | |
| Epilepsy | 16 | |
| Musculoskeletal | arthritis | 2 |
| fractured ankle | 1 | |
| bilat hip replacement | 1 | |
| spina bifida | 1 | |
| wheelchair bound-RTA | 1 | |
| Eyes | cataract operation | 1 |
| corneal ulceration | 1 | |
| congenital absent eyes | 1 | |
| ptosis | 1 | |
| glaucoma surgery | 1 | |
| long-sighted | 1 | |
| Ears | ear drum perforation | 2 |
| ear surgery | 1 | |
| grommet insertion | 1 | |
| Skin | eczema | 10 |
| psoriasis | 4 | |
| infections | 2 | |
| Endocrine | diabetes | 6 |
| anaemia | 4 | |
| Other | hare lip | 1 |
| None | 128 | |
| Unknown | 4 | |
A standard physical examination was undertaken, involving a detailed assessment of the person's height, weight, cardiovascular, respiratory, abdominal, genitourinary and neurological systems. Visual acuity was assessed using a graded picture test based on Snellen's chart described by Kay (Kay, 1983). An external examination of the eyes and ophthalmoscopy was undertaken to assess for cataracts, strabismus, keratoconus and nystagmus. Hearing acuity was assessed using whisper speech and distraction tests. Presence of cerumen was assessed by otoscopic examination. Venesection was performed for haematological, biochemical and thyroid status.
Results
Two-hundred and one adults with Down syndrome participated in this study, sex distribution being 102 (50.7%) males and 99 (49.3%) females. The mean age of the sample population was 42.22 years (standard deviation [SD] 12.51; standard error [SE] 0.88; range 16-76 years). The majority of the individuals were living in the community, with 73 (36.3%) living in supervised community units and 85 (42.3%) living in their family homes. Forty-three (21.4%) were resident in the hospital setting. Thirty-eight (18.9%) individuals had mild learning disability, 134 (66.7%) had moderate and 27 (13.4%) had severe impairment, and two were unknown.
Several past medical disorders were reported and these are given in Table 1. The commonest disorders were epilepsy, in 16 (8.0%) individuals, skin pathology in 16 (8.0%) subjects and respiratory problems in 16 (8.0%).
The majority of individuals, 138 (69%), were co-operative with the physical examination, but 45 (22%) were mildly unco-operative, requiring encouragement from carers and 18 (9%) were unco-operative with most part of the examination. Findings for medical problems of the sample population are given in Table 2.
The resting heart rate was measured for 190 (95.5%) subjects. The mean rate was 65 beats per minute (SD 5.19, SE 0.38, range 58-85). For males the mean value was 64 beats/min and for females 65 beats/min (no statistically significant difference, t-test=1.01; P=0.32). The rates were skewed towards the lower end of the normal distribution. The mean resting heart rate for the general population is 72 beats/min (range 60-100). The findings suggest adults with Down syndrome have lower resting heart rates than the general population (65:72).
| Finding | Sample size | Prevalence | ||
|---|---|---|---|---|
| N | % | |||
| Stature | 201 | All subjects below mean for non- learning disability population | ||
| Weight | 186 | |||
| -underweight | 13 | 7 | ||
| -overweight | 150 | 81 | ||
| -obese | 96 | 52 | ||
| Cardiovascular | 183-189 | |||
| -hypertension | 1 | |||
| -cardiac murmur | 23 | 12 | ||
| Respiratory disorders | 183 | |||
| -chest infection | 3 | 2 | ||
| Gastrointestinal disorders | 183 | |||
| -scars from previous surgery | 8 | 4 | ||
| Genitourinary disorders | 72 males | |||
| -undescended testis | 11 | 15 | ||
| -hypogenitalia | 4 | 6 | ||
| -other | 4 | 6 | ||
| Musculoskeletal disorders | 183 | |||
| -flat feet | 128 | 70 | ||
| -arthritis | 1 | |||
| -gout | 1 | |||
| -other | 4 | 2 | ||
| Dermatological disorders | 201 | |||
| -xerosis | 79 | 39 | ||
| -alopecia | 37 | 18 | ||
| -alopecia totalis | 5 | 3 | ||
| -eczema | 20 | 10 | ||
| Eyes/Vision | 192 | |||
| -poor vision | 27 | 14 | ||
| -severe impairment | 8 | 4 | ||
| -cataracts | 48 | 24 | ||
| -keratoconus | 19 | 10 | ||
| -nystagmus | 21 | 11 | ||
| Hearing | 193 | |||
| -poor hearing | 20 | 10 | ||
| -severe impairment | 3 | 2 | ||
| -cerumen | 38 | 20 | ||
| *Determined by body mass index - underweight = <21, overweight = >24, obese = >29 | ||||
Blood pressure measurements were available for 183 (93%) subjects. The mean systolic reading for the sample population measured was 115 mmHg (SD 13.1; SE 1.0, range 80-180) and a mean diastolic reading for the sample of 75 mmHg (SD 7.97; SE 0.59, range 50-100). No sex difference was found. There was a significant positive correlation between increase in age and increase in systolic and diastolic blood pressure readings (Pearson's product-moment coefficient 0.28; P<0.001 for systolic and 0.23; P<0.05 for diastolic; Figure 1). Seven individuals had diastolic readings over 90 mmHg and five individuals had systolic readings over 150 mmHg. However, there was only one case of hypertension (raised diastolic [>90 mmHg] and systolic [>140 mmHg]) with readings of 180/100 mmHg.
Blood pressure changes for the non-learning disabled population as determined by age (Hamilton et al, 1954) are also shown in Figure 1. Findings for the sample with Down syndrome show that mean diastolic and systolic blood pressures are below those of the non-learning disabled population (115/75:120/80). Also the increase in blood pressure with age is less marked for people with Down syndrome as compared to the non-learning disabled population.
Twenty-three (12.2%) of 189 individuals examined were found to have a cardiac murmur, but only one had associated heart failure. Virtually all murmurs were systolic in origin, except for one person with both diastolic and systolic murmurs. Of the 23 individuals with cardiac murmurs five (22%) had keratoconus. This is a statistically significant finding (Chi-squared test with Fisher's Exact probability, P<0.05).
Although occasional abnormalities were seen, no consistent significant pathology of the respiratory and abdominal systems was found. The commonest abnormality of the musculo-skeletal system was presence of flat feet (70%). Other occasional findings included one person with active arthritis of the knee, one person with gout of the large toe, another with longstanding abnormalities of leg size asymmetry and one person with congenital limb deformities. Neurological changes associated with dementia were seen, e.g. increased muscle tone, bed-ridden contractors but complications secondary to Atlanta-axial instability were not found.
The majority of subjects were overweight or obese. One hundred and fifty (81%) of those examined (N=186) had values of body mass index (weight/height x height; BMI) above the recommended level (>24). A degree of hair loss was seen in 37 (18.4%) of individuals. Five (2.5%) individuals had alopecia totalis. Excessive dry skin (xerosis) was seen in 79 (39.3%) of the sample, along with onychgrophosis in 40 (20%) subjects, unchomycosis in 10 (5%) and eczema 20 (10%) subjects.
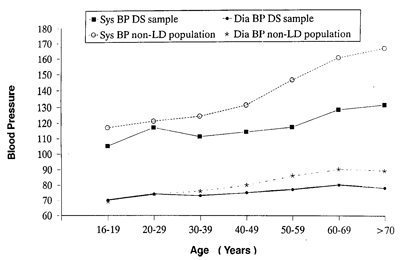
Figure 1. Blood pressure distribution for Down syndrome and non-learning disability population.
The genitalia were not examined in female subjects. This was thought by the author to be inappropriate and beyond the remit of this particular study. The external genitalia were examined in 72 of the 102 males in this study. Twenty were unco-operative with the examination and 10 carers refused permission for the examination. The majority had normal genitalia (53 [73.6%]) with the commonest abnormal findings of undescended testis (one or both) in 11 (15.3%) males, hypogenitalia in 4 (5.6%) and phimosis in two individuals. One individual had an inguinal hernia and another evidence of partial amputation of the penis for malignancy.
One-hundred and ninety-two (95.5%) individuals had visual assessments performed. The majority, 119 (62% of those examined) had no impairment of vision. Thirty-five (18.3%) had significant impairment of vision (moderate or severe) leading to a sensory loss. Of 193 (96%) individuals assessed for hearing function, over two-thirds had no detected impairment. Twenty-three (11.5%) had significant clinical impairment. Three (1.5%) cases were of severe hearing loss. One-fifth (19.7%) of the sample tested had moderate amount of cerumen present.
Haematological results were available for 147 (73.5%) of individuals. Of the 54 individuals who did not have results available, 39 (18.9% of the individuals) were unco-operative with venesection and 16 (8.0%) were co-operative but had failed venesection (no success after two attempts). The mean values for the different haematological parameters are given in Table 3.
| Variable | Mean Value (Normal value) | Significance | |
|---|---|---|---|
| Red blood cell count (RBC) | -males | 4.71 x 10 12 /1 (4.2-5.7 x 10 12 /1) | NS |
| -females | 4.37 x 10 12 /1 (3.8-5.1 x 10 12 /1) | NS | |
| Haemoglobin (Hb) | -males | 14.65 g/dl (13.4-17.0 g/dl) | NS |
| -females | 14.04 g/dl (11.4-15.0 g/dl) | NS | |
| Packed cell volume (PCV) | -males | 0.44 1/1 (0.40-0.50 1/1) | NS |
| -females | 0.43 1/1 (0.35-0.45 1/1) | NS | |
| Mean cell volume (MCV) | 99.28 fl (90-98 fl) | Significantly raised | |
| Mean cell haemoglobin (MCH) | -males | 32.29 pg (28-34 pg) | NS |
| -females | 32.36 pg (27-33 pg) | NS | |
| Mean cell haemoglobin concentration (MCHC) | 32.95 g/dl (30-35 g/dl) | NS | |
| Red cell distribution width (RDW) | 13.63% (10-17%) | NS | |
| Platelets | 218 x 10 9 /1 (150-400 x 10 9 /1) | NS | |
| White blood cell count (WBC) | 5.53 x 10 9 /1 (4.0-11 x 10 9 /1) | NS | |
| Neutrophil count | 1.95 x 10 9 /1 (2.0-7.5 x 10 9 /1) | Significantly low | |
| Lymphocyte count | 1.11 x 10 9 /1 (1.0-4.0 x 10 9 /1) | NS | |
| Monocyte count | 0.26 x 10 9 /1 (0.2-0.8 x 10 9 /1) | NS | |
| Eosinophil count | 0.10 x 10 9 /1 (0-0.4 x 10 9 /1) | NS | |
| Basophil count | 0.06 x 10 9 /1 (0-0.1 x 10 9 /1) | NS | |
| Large undifferentiated cells | 0.08 x 10 9 /1 (0-0.3 x 10 9 /1) | NS | |
| NS = not significant | |||
Thirty-one (21%) individuals had haematological abnormalities requiring further attention; ten had anaemia (haemoglobin below 13.4 g/dl for males and below 11.4 g/dl for females), twelve with evidence of polycythemia on full blood count (haemoglobin and packed cell volume above upper limits of normal range), two cases with evidence of concurrent infections (raised white blood cell counts) and seven with low platelet counts (below <150 x 10 9 /l). Twenty-nine individuals had low white blood cell counts (<4.0 x 10 9 /l) with significant neutropenia (mean 1.95 x 10 9 /l; normal range 2.0-7.5 x 10 9 /l). The mean MCV (mean cell volume) value for the sample with available results was 99.28 fl/l. A raised MCV (value of the MCV greater than 98.8 fl/l) was seen in 70 (47.9%).
Only three of the 10 cases with anaemia were known previously. Of those subjects with evidence suggestive of polycythemia, two individuals had clinically important findings, both of whom were being managed for their condition. Both cases with raised white blood cell counts were on antibiotics for chest infections. None of the individuals with low platelet counts had been investigated further.
One-hundred and fifty (75%) of the sample had biochemical results available (mean findings given in Table 4). As for haematological results some individuals were uncooperative with venesection and others had unsuccessful venesection. No consistent abnormality was found other than hypocalcaemia (calcium less than 2.20 mmol/l). The mean value for the sample was 2.19 mmol/l (normal range 2.20 - 2.26 mmol/l). Over half those tested (52%) had values below the lower limit of the reference range.
| Variable | Mean Value (Normal value) | Significance compared to non-LD population values |
|---|---|---|
| Albumin | 39.1 g/l (35-50 g/l) | NS |
| Bilirubin | 9.1 micromol/l (up to 22) | NS |
| Calcium | 2.19 mmol/l (2.20-2.65) | Significantly reduced |
| Creatinine | 98.1 micromol/l (50-120) | NS |
| Globulin | 33.6 g/l (20-35 g/l) | NS |
| Glucose | 4.95 mmol/l (3.0-8.0 mmol/l) | NS |
| Sodium | 139.0 mmol/l (135-145 mmol/l) | NS |
| Urea | 6.0 mmol/l (2.5-7.5 mol/l) | NS |
| Potassium | 4.4 mmol/l (3.5-5.0 mmol/l) | NS |
| Alkaline Phosphatase | 79.3 IU/l (70-350 IU/L) | Lower limit of normal |
Hypocalcaemia may be related to a low albumin but the mean albumin level for the sample was 39.1 mmol/l (normal range 36.0-48 mmol/l). Only 10% had levels below the normal reference range. However, a highly significant positive correlation between serum albumin and calcium was found (Pearson's product-moment coefficient 0.62; P<0.001).
Idiosyncratic abnormalities for the differing biochemical variables were found but only six individuals had findings of immediate clinical significance. Four cases had hyperglycaemia; all four were known diabetics receiving treatment, including regular medical input. These results show that their diabetes was poorly controlled. One person had known renal failure (raised creatinine and urea) and one person had raised alkaline phosphatase.
Thyroid function status was assessed in 160 subjects. Normal thyroid status (normal thyroxine [T4] and thyroid stimulating hormone [TSH]) was found in 104 (65%), subclinical hypothyroidism (normal T4, raised TSH) in 19 (11.9%) subjects and definite hypothyroidism (low T4, raised TSH) in 13 (8.1%) of subjects. Five (3.1%) subjects had biochemical evidence of hyperthyroidism (raised T4, low TSH).
Discussion
Physical disorders reported in adults with learning disabilities, with relatively high prevalence rates include, obesity (45% in the study by Wilson and Haire, 1990), sensory impairment (hearing 20%, ocular pathology 49% in study by Larson and Lapointe, 1986) and epilepsy (Jacobson and Janicki, 1985). In this study 81% of individuals examined were found to be overweight or obese (BMI >24), significant impaired vision was present in 18% and significant impaired hearing in 12% of those examined. A history of epilepsy was found in 8% of subjects. Overall, obesity appears to be particularly associated with Down syndrome, although other disorders are of a similar magnitude to those found in the learning disability population as a whole.
Although all the individuals in the study had normal resting heart rates, the mean heart rate for the sample (65 beats/min) was significantly lower than that for the non-learning disabled population (72 beats/min) and lower than previously reported for people with Down syndrome by Goldhaber et al. (1987) of 72+/-10 beats/min. The sample size in the study by Goldhaber et al. (1987) was only 35 individuals with a mean age of 26 years. This study had a sample size five times that of Goldhaber et al.'s study and with an older population. Few individuals presented with a tachycardia that may have been associated with anxiety associated with undergoing a physical examination.
The mean systolic blood pressure found was 115 mmHg and diastolic of 75 mmHg. Both readings were lower than those for the non-learning disabled population (120/80 mmHg). Goldhaber et al (1987) had reported values of 121 mmHg systolic and 72 mmHg diastolic for people with Down syndrome. Richards and Enver (1979) found blood pressure readings of 265 Down syndrome people to be significantly below that for age-matched non-learning disabled individuals. The finding of this study tend to support the findings of these latter researchers. Further, Richards and Enver (1979) found that blood pressure readings increased with age less dramatically in people with Down syndrome than in the non-learning disabled population. Results of this study again confirm these findings, blood pressure was found to be age-related in adults with Down syndrome but the rise with age was less marked than seen for the non-learning disabled population. Only one person had evidence of hypertension, suggesting people with Down syndrome may not be vulnerable to this disorder.
Twelve percent of the sample had cardiac murmurs, usually with no associated heart failure. Using echocardiography, Goldhaber et al. (1987) found a much higher prevalence of 71%. Without cardiological assessments using echocardiography it is not possible to say whether such murmurs are due to, as previously reported, to mitral valve prolapse or aortic valve regurgitation.
As reported by Howells in 1992, this study also found a significant association between the presence of a cardiac murmur and keratoconus (P<0.05). Such an association is probably due to connective tissue abnormalities, as similar to people with Marfan's syndrome.
Overall, these cardiovascular findings are clinically very important and suggest people with Down syndrome have significant differences to the non-learning disabled population. Adults with Down syndrome have a lower mean heart rate, lower age-specific blood pressures but a greater prevalence of cardiac valve pathology. The former findings suggest adults with Down syndrome have a lower risk for coronary heart disease but may be at greater risk of heart failure.
Although people with learning disabilities and Down syndrome may suffer from repeated upper respiratory infections and episodes of constipation, significant respiratory and gastro-intestinal findings in adults are uncommon. A prevalence of 7% for respiratory findings was reported by Minihan and Dean (1990) but no case of significant gastro-intestinal pathology. No individual with significant respiratory or gastro-intestinal pathology was found by Wilson and Haire (1990). In this study, upper respiratory infections were found in three adults with Down syndrome, supporting other research which found a low prevalence of serious pathology of the respiratory system in people with learning disabilities. No active gastro-intestinal pathology was found in the sample, although evidence of previous surgery was seen in eight (4%) subjects. These findings support the view that significant respiratory and abdominal pathology associated with Down syndrome are likely to be diagnosed and managed in children rather than in adulthood.
Both internal and external genitourinary abnormalities have been described in people with Down syndrome. In this study only external abnormalities of the male genitalia were examined. Female genitalia were not examined as this was thought by the author to be too intrusive for the remit of this study. As reported in previous studies (Smith and Berg, 1976; Benda, 1969) relatively common abnormalities found in this study included undescended testis and hypogenitalia. No clinical evidence of undiagnosed tumours was found.
An association between atlanto-axial and atlanto-occipital instability and Down syndrome is now well established (Pueschel et al, 1992; Maclachlan et al, 1993). Such an association has been reported using radiological examinations. Clinical presentation remains controversial with recent reports suggesting the risk of neurological complications secondary to the cervical instability has been over-represented (Cooke and Landsdale-Welfare, 1991). In this study neurological symptoms were present, but usually in the context of a dementing process. There was little evidence to suggest elderly subjects with Down syndrome had developed neurological complications secondary to cervical instability.
The reference ranges recited for the differing haematological and biochemical parameters apply to 95% of the non-learning disabled population. There is, therefore, a one in twenty chance of a result being 'abnormal.' Not surprisingly, in this study of 201 subjects the occasional finding was found to be outside the appropriate range.
Several haematological results required further assessment (anaemia, polycythemia, raised white blood cell count and low platelet count). Seven of the ten individuals with anaemia were unknown and required supplement therapy. Two of the 12 with polycythemia required medical intervention and both were receiving this. This also applied to the two subjects with raised white blood cell counts for chest infections, both being treated with antibiotics. None of the seven with low platelet counts had been investigated further.
Two haematological abnormalities consistently found for the sample population were increase in the mean red cell volume (macrocytosis) and low neutrophil count (neutropenia). The former is well recognised in people with Down syndrome (Akin, 1988, Wachtel and Pueschel, 1991). In this study approximately half of those tested (47.9%) had macrocytosis. The underlying cause of macrocytosis is unknown but is not in the vast majority of cases due to some other medical disorder e.g. vitamin B12 of folate deficiency.
Abnormalities in the neutrophil count in people with Down syndrome are known (Smith and Berg, 1976) but low blood counts for adults with Down syndrome have not been previously recognised. Further research is required to investigate the significance of a low neutrophil blood count.
As per haematological results, occasional abnormalities of biochemical parameters were found but the only significant finding for the sample as a whole was hypocalcaemia (mean 2.19 mmol/l). Over half of those tested had plasma calcium levels below the lower limit of the reference range (<2.20 mmol/l). Hypocalcaemia was positively associated with levels of plasma albumin (P<0.001). Although hypocalcaemia has been recognised in children and young adults with Down syndrome (Sobel et al, 1958; Stern and Lewis, 1958) it has not been reported in older individuals. The association with albumin has not been demonstrated previously. Further research is required to investigate the clinical significance of low plasma calcium in individuals with Down syndrome.
Four cases of hyperglycaemia were found, all known diabetics. As with thyroxine replacement therapy, close monitoring of anti-diabetic medication is required as the findings of this study suggested poor diabetic control.
This study, as reported previously, found a high prevalence of thyroid dysfunction (35%) in people with Down syndrome. However, this is the largest study of adults with Down syndrome to be reported and the first to investigate a significantly older population with Down syndrome. Subclinical hypothyroidism was found to be the commonest abnormality (11.9%), but a significant number had definite hypothyroidism (4%). No case of clinical hyperthyroidism was found.
As demonstrated by this study, adults with Down syndrome suffer from a high prevalence of physical disorders. Medically significant physical disorders include, sensory impairment, overweight and obesity and thyroid dysfunction. Individuals with Down syndrome may not be able to communicate any pain or discomfort associated with a given illness. Ill health may be masked and may result in missed or misdiagnosis of psychiatric and physical illness. Complications may follow, ultimately, proving to be fatal.
In order to ensure, therefore, that appropriate healthcare is provided to adults with Down syndrome, health services must be aware of the diagnosis, treatment and management of such medical disorders that occur in this population. An active screening programme must be implemented.
An effective provision of such a service is best provided by access to good quality primary healthcare, and regular contact with the learning disability services. Individuals themselves and their carers need to be educated about the health difficulties and disorders that need to be observed. Better liaison between the general hospital services and psychiatric services with possibly joint assessments could prove the way forward.
Healthcare provision does need to be improved for people with Down syndrome and people with learning disabilities as a whole. This may involve employing staff with different skills to assess any given morbidity, to maximise the individual's own skills and to ensure that a high level of services is provided by carers who are also given support. Regular assessments from medical staff is a prerequisite.
With improved life expectancy of people with Down syndrome, older individuals are more vulnerable to physical, sensory and psychiatric morbidity. The development of a high quality comprehensive service is essential to ensure a good quality of life.
Glossary
- Acuity: Sharpness (of vision).
- Alopecia totalis: Complete absence of hair.
- Atlanto-axial instability/atlanto-occipital instability: X-ray examinations of the neck which are claimed to be associated with instability of the upper vertebrae of the neck.
- Cerumen: Ear wax.
- Contractures: Shortening of muscles due to fibrous change.
- Creatinine and urea: Substances which are measured in the blood as tests of kidney function.
- Cytogenetically: Related to genetic structure of the cell.
- Diastolic: That part of the blood pressure associated with the relaxation of the ventricles.
- Echocardiography: The use of sound waves to investigate the heart.
- Hyperglycaemia: High blood sugar.
- Hypocalcaemia: Low blood calcium.
- Inguinal (hernia): A protrusion of part of the bowel through a gap in the lower abdomen.
- Keratoconus: Abnormal conical shape of the cornea of the eye.
- Marfan's syndrome: An inherited disorder characterised by long fingers and toes, defects to the heart and eyes.
- Mean cell volume: An expression of the size of the red blood cell.
- Morbidity: The state of being diseased.
- Neutropenia: Decrease in the number of neutrophils in the blood.
- Neutrophil: A form of white cell which kills bacteria.
- Nystagmus: Rapid short movements of the eye.
- Onychogryphosis: Abnormal thickening of the nail.
- Ophthalmoscopy: Examination of the retina of the eye.
- Otoscopic: To do with the ear.
- Packed cell volume: An expression of the amount of haemoglobin in the blood.
- Phimosis: Narrowing of the opening of the foreskin.
- Phosphatases: A group of enzymes which may be measured in the blood.
- Polycythemia: An increase in the haemoglobin concentration of the blood.
- Strabismus: Squint.
- Symptomatology: The symptoms of disease.
- Systolic: That part of the blood pressure associated with the contractile phase of the heart.
- Tachycardia: Rapid heart beat.
- Thyroxine replacement therapy: Treatment with the thyroid hormone.
- Unchomychosis: Disease of nails of fingers and toes.
- Venesection: Taking a blood sample from a vein.
- Xerosis: Abnormal dryness of eyes, skin or mucous membranes.
References
- Akin, K. (1988). Macrocytosis and leukopenia in Down syndrome. Journal of the American Medical Association, 259, 842.
- Baird, P.A. and Sadovnick, A.D. (1988). Life expectancy in Down syndrome adults. Lancet, 2, 1354-1356.
- Benda, C.E. (1969). Down syndrome: Mongolism and its Management (rev. ed.). New York: Grune and Stratton.
- Burt, D.B., Loveland, K.A. and Lewis, K.R. (1992). Depression and he onset of dementia in adults with mental retardation. American Journal on Mental Retardation, 96, 502-511.
- Caputo, A.R., Wagner, R.S., Reynolds, D.R., Guo, S. and Goel, A.K. (1989). Down syndrome. Clinical review of ocular features. Clinical Pediatrics, 28, 355-358.
- Collacott, R.A., and Cooper, S.-A. (1992). Adaptive behaviour after depressive illness in Down syndrome. The Journal of Nervous and Mental Disease, 180, 468-470.
- Cooke, L.B., and Lansdall-Welfare, R. (1991). Atlanto-axial instability in adults with Down syndrome-A survey of a long-stay hospital population. West of England Medical Journal, 106, 7-8.
- Department of Health. (1992) The Health of the Nation; A Strategy for Health in England. London: HSMO, 1992 (Cm. 1986).
- Dinani, S. and Carpenter, S. (1990). Down syndrome and thyroid disorder. Journal of Mental Deficiency Research, 34, 187193.
- Evenhuis, H.M., van Zanten, A., Brocaar, M.P. and Roerdinkholder, W.H.M. (1992) . Hearing-loss in middle-aged persons with Down syndrome. American Journal on Mental Retardation, 97, 47-56.
- Goldhaber, S.Z., Brown, W.D., and St. John Sutton, M.G. (1987). High frequency of mitral valve prolapse and aortic regurgitation among symptomatic adults with Down syndrome. Journal of the American Medical Association, 258, 1793-1795.
- Hamilton, M., Pickering, G.W., Roberts, J.A.F. and Sowry, G.S.C. (1954). The aetiology of essential hypertension. 1. The arterial pressure in the general population. Clinical Science, 13, 11-16.
- Hestnes, A., Sand, T., and Fostad, K. (1991). Ocular findings in Down syndrome. Journal of Mental Deficiency Research, 35, 194-203.
- Howells, G. (1986). Are the medical needs of mentally-handicapped adults being met? Journal of the Royal College of General Practitioners, 36, 449-53.
- Jacobson, J.W. & Janicki, M.P. (1985). Functional and health status characteristics of persons with severe handicaps in New York state. The Journal of The Association for Persons with Severe Handicaps 10, 51-60.
- Kay, H. (1983). New method of assessing visual acuity with pictures. British Journal of Ophthalmology, 67, 131-133.
- Larson, C.P. and Lapointe, Y. (1986) The Health Status of mild to moderate intellectually handicapped adolescents. Journal of Mental Deficiency Research, 30, 121-128.
- Maclachlan, R.A., Filder, K.E., Yeh, H., Hodgetts, P.G., Pharand, G. and Chau, M. (1993) . Cervical spine abnormalities in institutionalised adults with Down syndrome. Journal of Intellectual Disability Research, 37, 277-285.
- Minihan, P.M., and Dean, D.H. (1990). Meeting the needs for health services of persons with mental retardation living in the community. American Journal of Public Health, 80, 1043-1048.
- Oliver, C. and Holland, A.J. (1986). Down syndrome and Alzheimer's disease: a review. Psychological Medicine, 16, 307-322.
- Prasher, V.P. (1993). Longevity and Down syndrome. British Journal of Psychiatry, 161, 722.
- Prasher, V.P. and Krishnan, V.H.R. (1993). Age of onset and duration of dementia in people with Down syndrome. International Journal of Geriatric Psychiatry, 8, 923-927.
- Pueschel, S.M. & Pezzullo, J.C. (1985). Thyroid dysfunction in Down syndrome. American Journal of Diseases of Children, 139, 636639.
- Pueschel, S.M., Scola, F.H. & Pezzullo, J. (1992). A longitudinal study of atlanto-dens relationships in asymptomatic individuals with Down syndrome. Pediatrics, 89 1194-1198.
- Richards, B.W. and Enver, F. (1979). Blood pressure in Down syndrome. Journal of Mental Deficiency Research, 23, 123-135.
- Smith, G.F. and Berg, J.M. (1976). Down Anomaly (2nd ed). Edinburgh: Churchill Livingstone.
- Sobel, A.E., Strazzulla, M., Sherman, B.S., Elkan, B., Morgenstern, S.W. et al. (1958) . Vitamin A absorption and other blood composition studies in mongolism. American Journal of Mental Deficiency Research, 62, 642.
- Stern, J. and Lewis, W.H.P. (1958). Calcium, phosphate and phosphatase in mongolism. Journal of Mental Science, 105, 1012.
- Wachtel, T.J., and Pueschel, S.M. (1991). Macrocytosis in Down syndrome. American Journal of Mental Retardation, 95, 417-420.
- Wilson, D.N., and Haire, A. (1990). Health care screening for people with mental handicap living in the community. British Medical Journal, 301, 1379-1381.
- World Health Organisation (1992). The ICD-10 Classification of Mental and Behavioural Disorders. Clinical Descriptions and Diagnostic Guidelines. Geneva: WHO.
- Yeates, S. (1992). Have they got a hearing loss? A follow-up study of hearing in people with mental handicaps. Mental Handicap, 20, 126-133.

